Surgical Technique Guide for Distraction Bridge Plating of Distal Radius Fractures
Douglas P. Hanel, MD
Professor of Orthopaedics and Sports Medicine
Director of Orthopaedic Education
University of Washington Medical Center
Seattle, WA
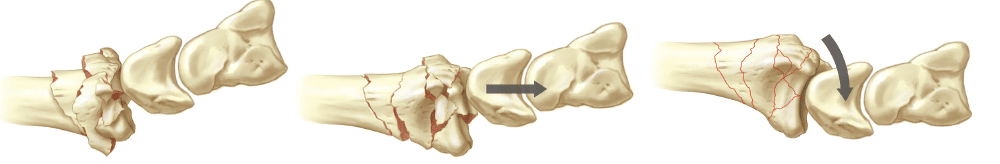
Longitudinal traction is used to assess the benefits of ligamentotaxis for restoration of the articular surface. Finger traps are applied to the index and middle fingers with 10 lbs. of traction off the end of the table. Under fluoroscopy the Agee closed reduction maneuver is performed; a combination of longitudinal traction and palmar translation to restore radial length, inclination and sagittal tilt. This maneuver will reveal the integrity of the volar ulnar corner of the radius. Finally, pronate the hand to correct the supination deformity.
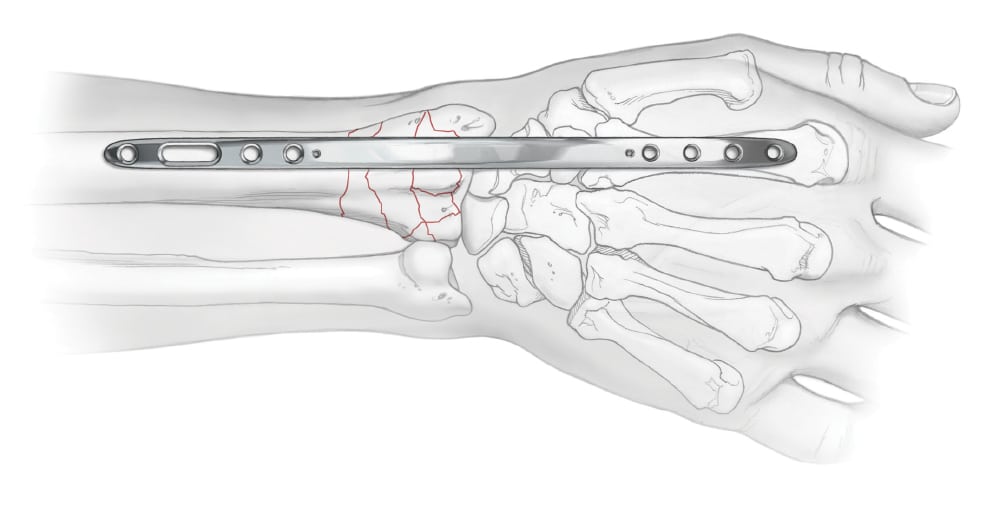
The plate is superimposed over the radial diaphysis to the metadiaphysis of the second metacarpal, and verified with a C-arm. Mark the skin at the level of the proximal and distal screw holes. The subcutaneous tissues are infiltrated with 0.25% bupivacaine with epinephrine to promote hemostasis. A tourniquet is not routinely used.
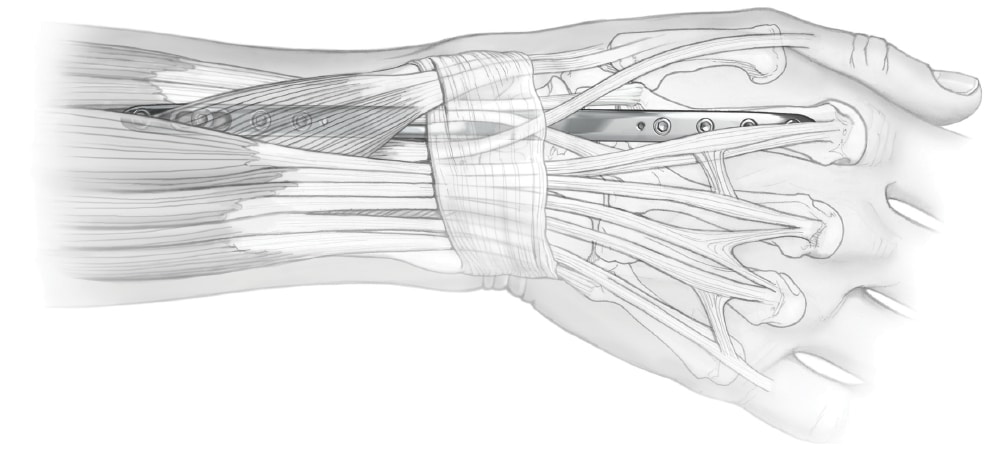
A 5-7 cm incision is made at the base of the 2nd metacarpal and continued along the shaft. The insertions of the extensor carpi radialis longus (ECRL) and the extensor carpi radialis brevis (ECRB) are identified as they pass beneath the distal edge of the second dorsal wrist compartment to insert on the 2nd and 3rd metacarpal bases, respectively
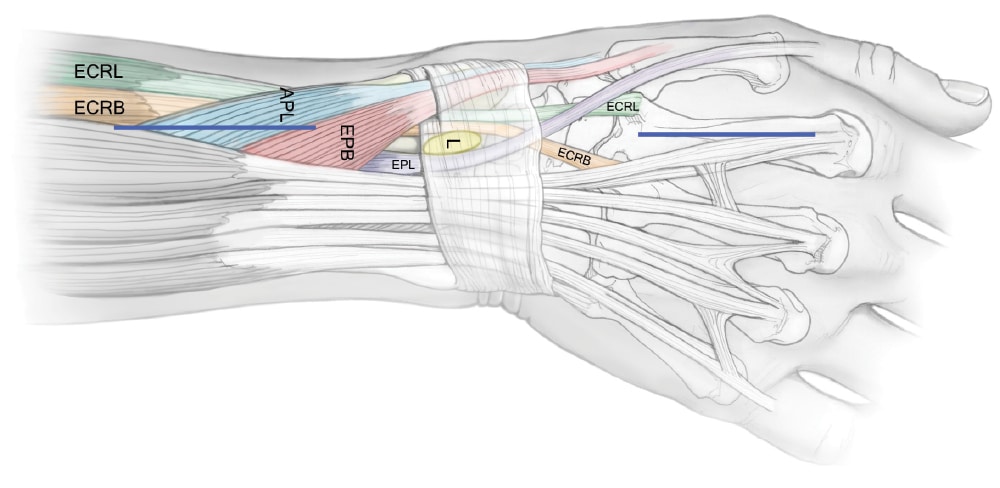
A second incision is made just proximal to the outcropper muscle bellies of the abductor pollicis longus (APL) and the extensor pollicis brevis (EPB), in line with the ECRL and ECRB tendons. The interval between the ECRL and ECRB is developed, and the diaphysis of the radius is exposed. A third, or periarticular, incision may also be used to assess, reduce and stabilize the articular surface.
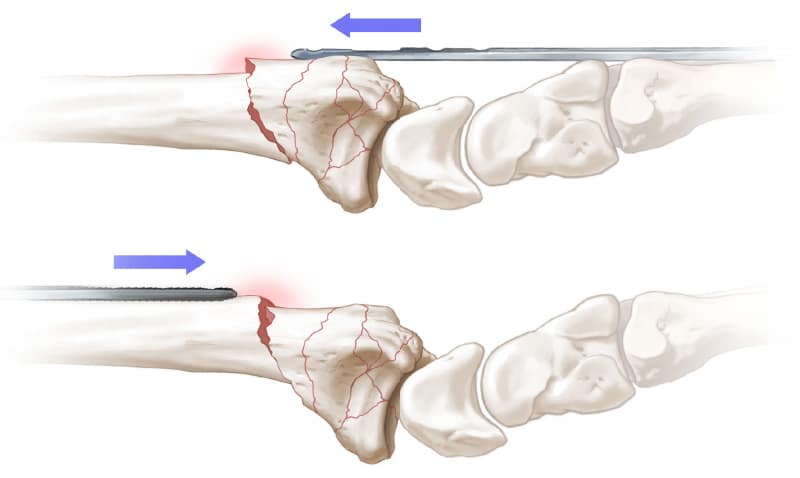
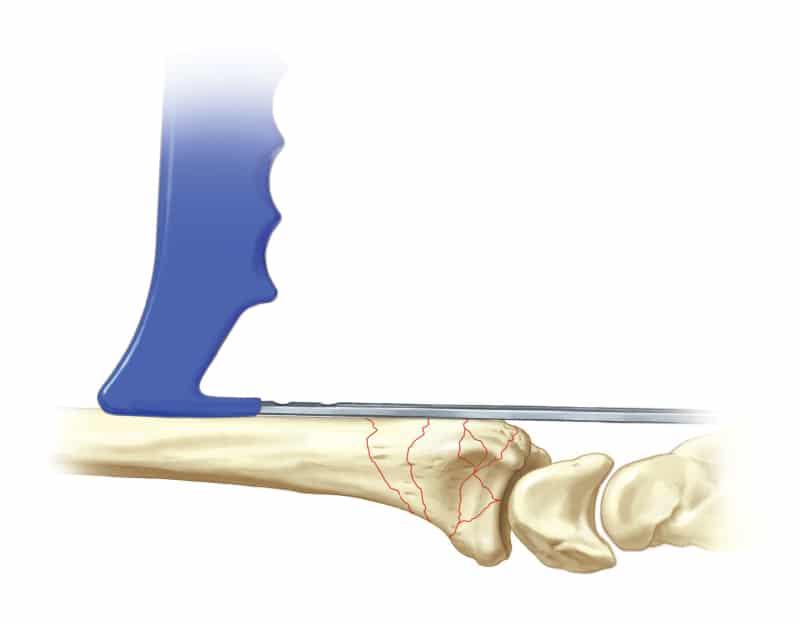
Consider the direction of carpal displacement before inserting the plate. This avoids catching the plate on or under fracture fragments as it is advanced.
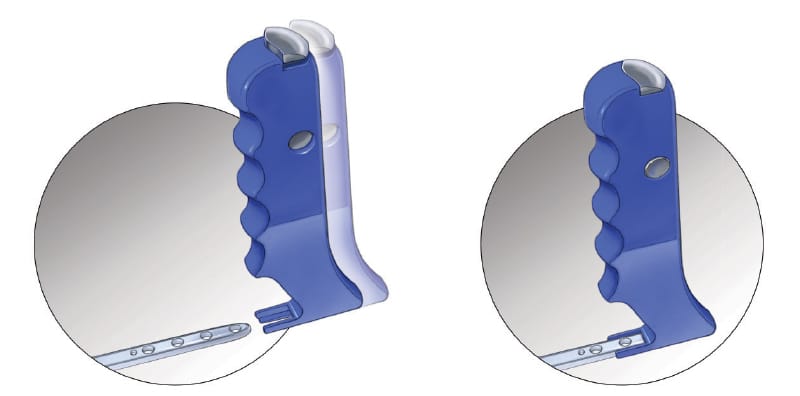
Depending on the direction of insertion, the handle can be locked onto either end of the plate.
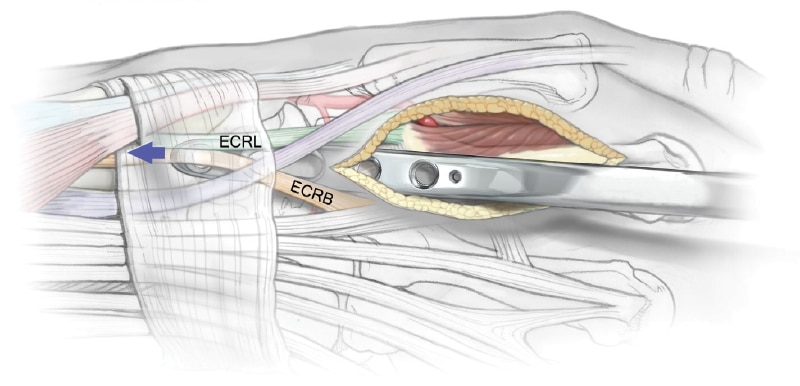
Typically, the plate is passed proximally through the 2nd compartment. Alternatively, the plate can be inserted proximally beneath the muscle bellies of the outcroppers extraperiosteally and advanced distally between the ECRL and ECRB tendons. Some resistance will be encountered, but this can be overcome with gentle manipulation of the handle.
After passing the plate, it is then secured to the 2nd metacarpal by placing a non-locking 2.7mm cortical screw through the most distal hole. The proximal end of the plate is then identified in the forearm. If the radial length has not been restored, then the plate is pushed distally with the handle until the length is reestablished.
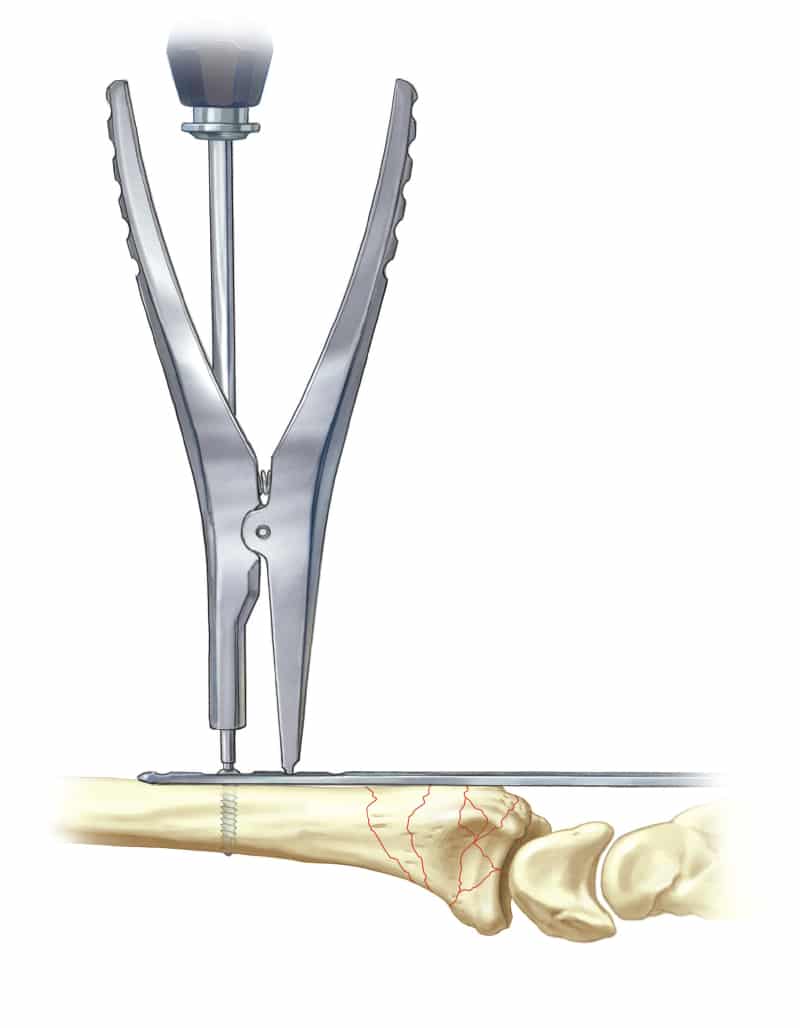
With a wrist in neutral rotation, and the plate aligned on the metacarpal and radial shafts, a non-locking 3.2mm cortical screw is placed into the distal end of the slotted hole to allow for additional distraction with the expander tool. The remaining holes are secured with locking or non-locking screws inserted with bicortical purchase.
Intra-articular reduction may be further adjusted by using limited periarticular incisions to allow: direct manipulation of articular fragments; placement of subchondral bone graft; repair of intercarpal ligament injuries; and augmentation of fractures with K-wires, Buttress Pins, Hook Plates or Pin Plates. Displaced volar ulnar corner fragments that are not reduced with the Bridge Plate alone require buttress support.
The DRUJ is assessed and if stable, then the limb is immobilized in a long arm splint with the forearm in 60° of supination for the first 10-14 days. If unstable, then repair or reconstruction of the DRUJ and triangular fibrocartilage complex is undertaken. In rare instances where the patient’s condition does not allow prolonging the operation, manually reduce the ulnar head into the sigmoid notch and pass at least two 1.6mm K-wires through the ulna into the radius proximal to the DRUJ.
Postoperative Rehabilitation:
Digit range of motion exercises start within 24 hours. Load bearing through the forearm and elbow is allowed immediately, as well as the use of a platform crutch when the patient is physiologically stable. At 1 month postoperatively the platform is removed and weight bearing is allowed through the hand grip of regular crutches. Lifting and carrying is restricted to approximately 10 lbs. until the fracture has healed.
DRUJ stability and forearm motion are assessed at 2 weeks. If the patient can supinate the forearm with little effort and the DRUJ is stable, then splinting is discontinued. Axial loading through the extremity is allowed for transfers and all weight-bearing needs. If supination is difficult or if the DRUJ was reconstructed acutely, then a removable long arm splint is fabricated. If the DRUJ was transfixed with K-wires, then the wires are removed on the third postoperative week and DRUJ stability is reassessed. Supplemental K-wires for articular fixation are removed 6 weeks postoperatively. The plate and screws are removed usually no earlier than 12 weeks after injury.
Clinical Pearls:
At the time of hardware extraction the screws are removed and the plate slid from the incision. If resistance is encountered, then axially twist the plate 720 degrees to break up any soft tissue adhesions and callus that grow around edges of the plate. This maneuver is not usually required when the smooth-edged stainless steel plates are used. A removable short arm splint is worn for 2 to 3 weeks after plate removal. Hand therapy at this point is directed at regaining motion and strength.
Disclosure: The author did not receive any outside funding or grants in support of this work. Neither he nor a member of his immediate family received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity.