Surgical Technique Guide STT Fusion
Mark S. Rekant, M.D.
Clinical Associate Professor
Department of Orthopaedic Surgery at Thomas Jefferson University
The Philadelphia Hand Center, P.C.
Philadelphia, PA
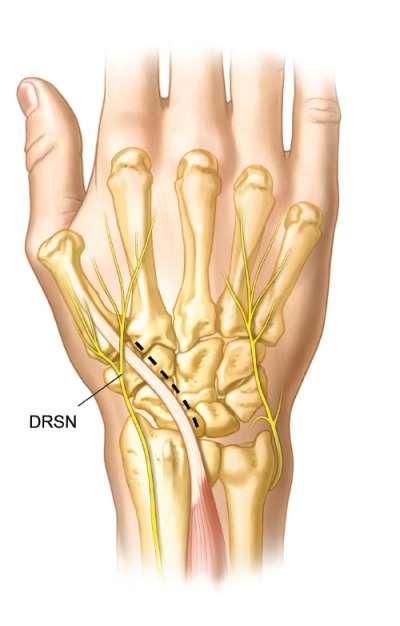
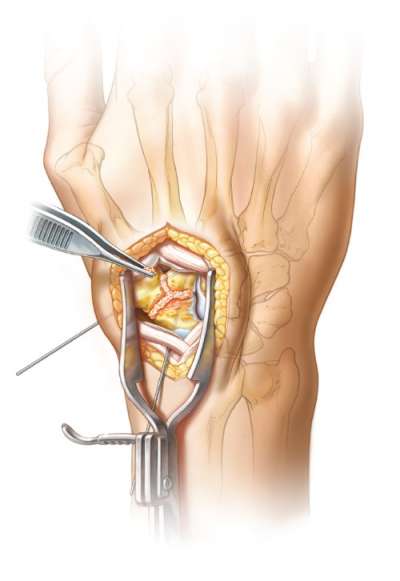
A dorsal longitudinal incision is made over the wrist in line with the scaphotrapeziotrapezoid (STT) joint, extending proximally in line with the extensor pollicis longus (EPL) to Lister’s tubercle. Skin flaps are elevated, and the dorsal sensory branch of the radial nerve (DRSN) is protected.
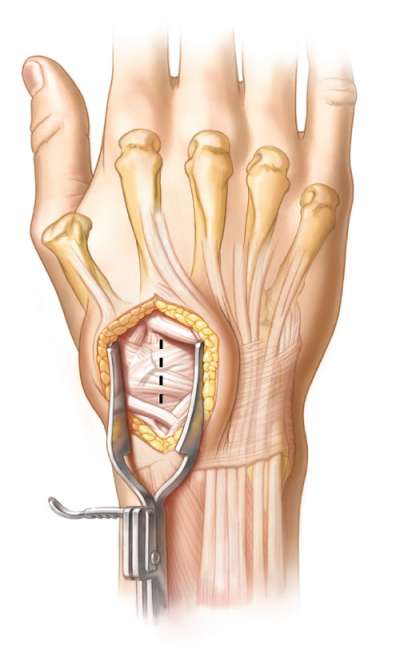
The extensor retinaculum is incised and released distal to Lister’s tubercle.
The EPL is retracted radially, while the 2nd extensor compartment tendons – extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB) – are retracted ulnarly.
If the scaphoid is subluxed, reduction to normal anatomical position is facilitated by a small periosteal elevator under the distal pole of the scaphoid.
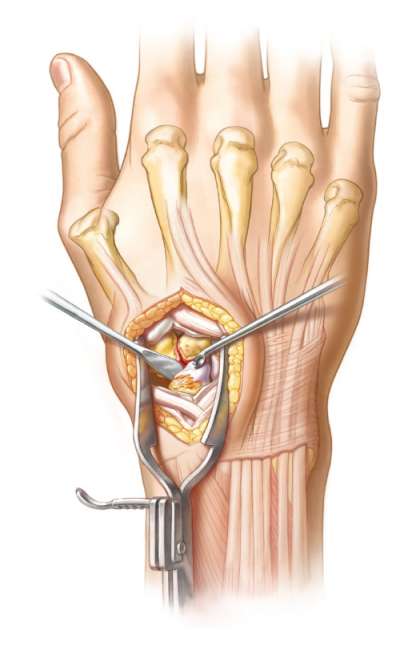
Once reduced to normal anatomical position, fusion sites are prepared. This is the most important part of the procedure. Meticulously decorticate cartilage of the scaphoid-trapezium-trapezoid joints.
A scalpel, curette, rongeur, osteotome or high speed burr can be used to denude the cartilage between the three bones, down through subchrondral bone to bleeding cancellous bone. To achieve optimal cancellous bone contact for fusion, denuding of the cartilage is carried down to the volar aspect of the STT joint.
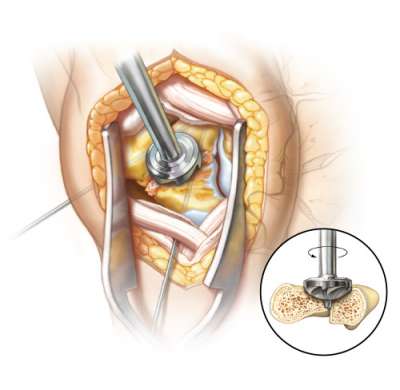
Provisional K-wire fixation maintains the reduction, provides resistance while using a reamer, prevents toggling of the bones and produces a more uniform surface area for the plate and screw placement.
To maintain reduction of the STT construct, one 0.045” K-wire is inserted from the scaphoid through the trapezoid. A subsequent 0.045” K-wire is placed from the trapezium through the trapezoid. Ensure K-wires are positioned volar enough to remain below intended reamed cavity.
If further reduction is required, a third K-wire can be inserted through the trapezium exiting the proximal pole of the scaphoid.
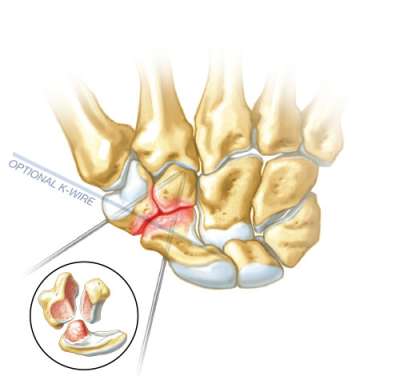
Autologous cancellous bone graft is taken from either Lister’s tubercle or elsewhere. The graft is packed between each of the joint surfaces to be fused and at the junction of the STT fusion down through the volar aspect. It is noteworthy that no bone graft has extruded into the scaphocapitate joint surface.
With bone graft packed into all interstices, confirm STT alignment and stability before reaming.
The reamer is centered over the junction of the STT joint to ensure all three bones are reamed equally. The reaming cavity must be at least flush with or slightly recessed below the surface of the dorsal aspect of the carpus.
It is important the plate is at least flush or slightly recessed relative to the level of the remaining dorsal carpal cortex.
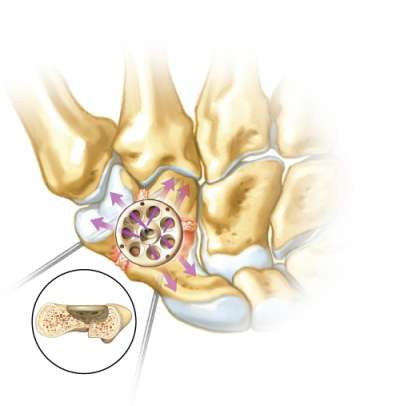
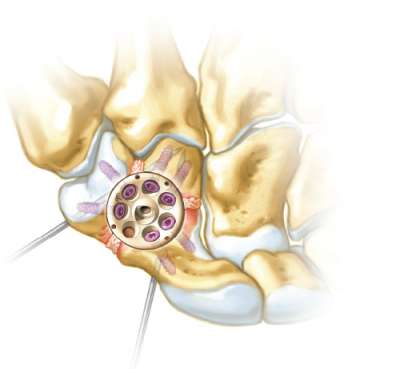
Rotate Fusion Cup for optimal alignment, allowing for two screws into each of the STT bones. Drill, measure and insert screws, but do not completely tighten until all screws have been inserted. Alternately tighten screws that are opposite to each other.
All screws are tightened and locked in a balanced fashion, with the screw head just flush with the Fusion Cup. Care is taken to avoid excessive volar screw threads.
Once all screws are placed, final intra-operative fluoroscopic images are obtained in multiple planes. Proper screw depth and placement should not violate the first carpometacarpal joint or the capitate articulation. Range of motion testing is also performed to ensure stability and proper positioning.
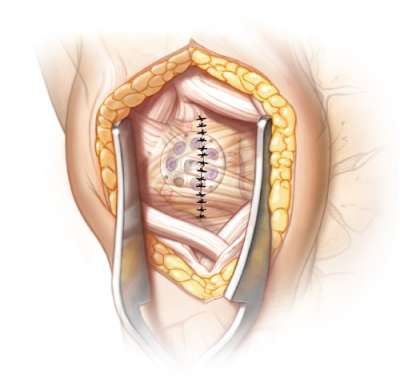
The capsule and/or retinaculum flap is repaired with absorbable sutures after copious amounts of irrigation. Hemostasis is assured. The skin is repaired. A short arm thumb spica splint is placed.
Disclosure: The author did not receive any outside funding or grants in support of this work. Neither he nor a member of his immediate family received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity.